Understanding & Addressing Trends in Physician & Nurse Burnout 2024
22 January 24
| Connor Bice & Miles Hepworth
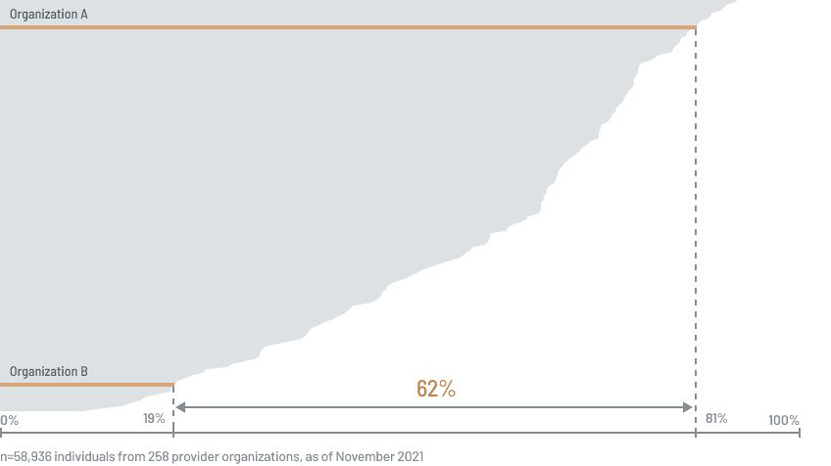
Key Findings See deeper insights on how to alleviate burnout Though burnout rates remain higher than pre-pandemic levels, they are beginning to stabilize for some and slightly decline overall Over the years, staffing shortages have been increasingly mentioned as a contributor to burnout, emerging as the top contributor to burnout in this report Those who are starting to feel burned out cite efficiency-related issues as reasons, while those who are completely burned out cite concerns related to the organization more broadly (e.g., lack of alignment from leadership) It is easier to prevent burnout by increasing EHR efficiency early on than it is to reduce burnout after it has already peaked Severity of clinician burnout and likelihood of leaving their organization are strongly correlated To alleviate burnout, both physicians and nurses want improved staffing and better alignment from leadership; physicians also want improved EHR efficiency, and nurses want better pay Burnout Rates for Physicians & Nurses Have Decreased since 2022; Prevalence of Burnout Differs across Organization Types The number of respondents reporting burnout (i.e., they chose one of the following responses: definitely burning out, symptoms of burnout won’t go away, or completely burned out) has slightly decreased since 2022. This is likely attributable to health systems implementing initiatives that combat burnout—for example, groups that foster community and belonging, efforts to reduce stigma around discussing burnout and mental health, and burnout reduction programs (led by chief wellness officers) that provide resources beyond what is provided by an EAP (employee assistance program). Still, burnout remains above pre-pandemic levels and is experienced by clinicians regardless of what EHR they use or what organization they work for. Across work environments, burnout is fairly consistent; however, it differs across organization types. Physicians and nurses working in community health systems are the most burned out, likely because these organizations experience higher turnover rates that result in increased workloads and less support (see the Yuma Regional Medical Center case study below to learn how one community health system is combating burnout). Clinicians at academic medical centers are the second-most burned out, as these organizations have more-complex workflows that decrease EHR efficiency and increase stress and after-hours documentation. Clinicians at FQHCs say their burnout is lower because of their intrinsic desire to help at-risk populations and their willingness to tackle uncomfortable situations. Clinicians at non-US health systems report the lowest burnout, saying regulatory pressures are less intense outside of the US. Physicians & Nurses Feel Overworked Due to Staffing Shortages & Inefficient Workflows In general, physicians and nurses feel they are overworked, and those experiencing symptoms of burnout report multiple contributors. Staffing shortages are the most-selected contributor for both physicians and nurses (particularly those at community health systems) and, over the past few years, have been cited increasingly more often as a contributor. Overall, top-mentioned contributors relate to either clinicians’ sense of belonging and appreciation—i.e., lack of teamwork and lack of shared values with leadership—or they relate to inefficiencies—i.e., EHR inhibiting efficiency and clinicians not having control over their workload. Furthermore, the contributors often perpetuate each other. When there aren’t enough staff members to support patients, physicians and nurses must shoulder a greater workload that can persist after hours, making it difficult to escape work stressors. Of note, the EHR is cited significantly less often than other burnout contributors. Physicians are more likely to mention it than nurses, especially since it can impede their efficiency. Still, the presence of an EHR doesn’t inherently lead to burnout and can even help mitigate burnout by improving efficiency and reducing duplicative work (view the Sutter Health case study and the Scripps Health case study for success stories). Burnout Contributors Shift Depending on Respondents’ Degree of Burnout; Organizations Can Prevent Severe Burnout by Improving EHR Efficiency & Reducing Workloads Physicians who are starting to feel burned out often cite no control over workload and a chaotic work environment as contributors. In contrast, those who are completely burned out cite no control over workload, lack of autonomy, and lack of shared values with leadership. Nurses who are starting to feel burned out most often cite staffing, while those who are completely burned out cite similar contributors to physicians who are completely burned out. Burnout contributors are easier to manage when physicians and nurses are experiencing early levels of burnout, rather than full burnout. To help alleviate clinician burnout in its early stages and improve EHR satisfaction, health systems can focus on improving efficiency—e.g., provide additional EHR education, support EHR personalizations, and decrease repetitive actions. Additionally, removing constant, daily irritants is an effective way to help both physicians and nurses feel more in control of their workload. Organizations frequently dismiss small concerns like these, encouraging users to find workarounds. But eventually, these irritants can build clinician’s frustration to an overwhelming point (click here to learn how Corewell Health—previously Spectrum Health—addressed this issue for their nurses). Organizations can prevent burnout and other challenges from worsening if they intervene early on, but addressing later-stage burnout is still feasible by realigning leadership’s values with clinicians’ and changing the organizational culture to be more inclusive and accepting of clinician feedback. Both physicians and nurses need evidence that the organization values their ideas. When addressing late-stage burnout, the leadership’s role is especially critical; if clinicians do not trust their leaders, solutions that worked before may no longer have the desired impact. In addition, previous KLAS research shows a correlation between strong IT delivery and reduced burnout. When clinicians perceive their IT team as partners who effectively reduce inefficiency, trust flourishes and burnout decreases (for more, see the Provider Burnout and the EHR Experience report and the Clinician Turnover and the EHR Experience report ). Arch Collaborative Case Study: Yuma Regional Medical Center Yuma Regional Medical Center, a member of the Arch Collaborative, proactively created a psychologist-led program to address physician burnout. Their strategy includes ongoing monitoring and follow-up appointments, fostering a culture of open communication, and reducing stigma around burnout. For more details, click here . Arch Collaborative Case Study: SUNY Upstate Medical University SUNY Upstate Medical University, a member of the Arch Collaborative, had their chief wellness officer lead a training program (EPIC4Me) that reduced after-hours documentation by 10%. This has significantly boosted efficiency for clinicians, thus reducing burnout. For more details, click here . Severity of Clinician Burnout & Likelihood of Leaving the Organization Are Strongly Correlated Burnout can be costly for an organization. One study shows that burned-out physicians are less productive and that organizations can experience an $80,000 decrease in revenue for every physician who is burned out. Unsurprisingly, it is in every organization’s best interest to save on costs by increasing staff satisfaction and limiting turnover; however, physicians and nurses can only tolerate burnout up to a certain point before deciding to leave their organization. The greater their burnout, the more likely they are to leave their organization within the next two years (physicians who indicate they are very likely to leave their organization are 15 times more likely to actually leave). The resulting turnover can force even more work onto the overburdened staff who remain. However, experiencing burnout doesn’t mean a physician or nurse will immediately make plans to leave, so organizations can reduce staff turnover by addressing burnout in its earlier stages. To Alleviate Burnout, Both Physicians & Nurses Want Improved Staffing & Better Alignment from Leadership; Physicians Also Want Improved EHR Efficiency while Nurses Want Better Pay Both physicians and nurses say the number-one way to alleviate burnout is to improve staffing , which includes decreasing expected workloads and hiring more staff. Both groups are overwhelmed by their list of tasks and feel like they can’t accomplish everything due to increased patient panels, excessive bureaucratic tasks, inefficient workflows, and reduced staffing. As previously mentioned, many of these concerns relate to the inefficiencies that drive early burnout among physicians and nurses. The more clinicians work after hours, the greater their burnout becomes. It is important for leaders to listen to clinicians’ concerns; if no action is taken, burnout can worsen and prompt clinicians to look elsewhere for work. The second most-mentioned way to alleviate burnout for physicians and nurses is better-aligned leadership . Many respondents say they need their leadership team to listen to and acknowledge concerns, and some worry their leaders are starting to focus more on finances than on their staff or even their patients. Physicians and nurses are resilient and can work in challenging situations; however, when there is misalignment with leadership and when physicians/nurses no longer feel supported or valued, the resulting negative sentiments can quickly lead to burnout. The third most-mentioned way to alleviate burnout differs between physicians and nurses: physicians want improved EHR efficiency while nurses want better pay . Regarding EHR efficiency, physicians (and some nurses) report they are increasingly doing more work with fewer resources. If organizations are unable to hire more staff to distribute the workload, they can instead ensure clinicians receive ample EHR education and that their workflows are optimized. Regarding pay, nurses (and some physicians) indicate that increased pay would help retain staff. Many nurses who have worked at their organizations for a long time believe they are less valued than contracted or travel nurses, who—despite working only temporarily at the organization—receive greater pay. KLAS Reports That Can Help Improve EHR Efficiency & Reduce Early-Stage Burnout Reducing physician and nurse burnout in the early stages is critical, and the best way to intervene is by improving efficiency. View the following KLAS reports for more information: Self-Directed eLearning 2023 : Additional EHR education can greatly increase time savings. This report explains that clinicians can save up to 90 minutes per week for every hour they spend engaged in eLearning. Personalizing the EHR 2023 : This report shares that physicians who adopt personalization tools, particularly templates, are able to close their charts significantly faster than those who do not adopt these tools. Clinician EHR Efficiency Software and Services 2023 : Healthcare delivery organizations don’t need to solve inefficiencies on their own. This report validates various vendor and services firm offerings that can help organizations improve EHR efficiency. Improve Staffing ”Decrease the bureaucratic workload that comes with the pseudo patient safety and quality improvement training, and provide better staffing . The root problem isn’t lack of training, and that’s a good thing. Instead, the root problem is the lack of support and the added workload , like documentation time during daily work hours. The decision makers know what they should do, but they have an agenda that is different from the providers’ needs.” —Physician “ Appropriately staff the floors with both RNs and techs, and ensure we have proper resources available so that patients don’t take out their frustration on staff when certain procedures are only available at certain times. Things like that really help eliminate extra stressors on the job.” —Nurse Align Leadership with Physicians/Nurses “Listen to physicians and fulfill their needs. The lack of accountability from leadership is astounding. There is also a clear problem with transparency between the medical group, which is only interested in finances, and the institution that purportedly values high quality and complex care. Fix leadership and support physicians adequately .” —Physician “ Take action when staff members speak up about problems in the office . I often think about leaving because there is no action and I feel as if my voice doesn’t matter. I feel like I work hard for others not to work at all. Often, I am assigned a task because other coworkers won’t complete theirs. There is no discipline for them, so I get stuck with the burnout.” —Nurse “The culture within my department has become increasingly toxic over the years. The clinical environment is becoming more chaotic, with more near-misses and less support staff, and the leadership is doing nothing to alleviate the situation. Despite being told repeatedly that clinics are not adequately staffed, the leadership does nothing to improve the situation .” —Physician Improve EHR Efficiency & Provide Better Pay Improve EHR Efficiency “My pain points are (1) the amount of work I take home and the amount of administrative work I do during non-clinical days, with the added bonus that all administrative work is uncompensated, (2) the out-of-control in-basket that I cannot keep up with, (3) poor access to my patients because my schedule is filled up with other people’s patients, and (4) the fact that the panel size is too large and still growing, resulting in us seeing an average of six to eight new patients per day.” —Physician “I have help outside the organization and appreciate the support provided, but the constant push to do more with less is relentless, and the organization needs to figure out a way to make it stop . We can all clearly see the unsustainability, yet we blithely march on. We are supposed to increase production while being given additional tasks due to understaffing and without getting additional help, and we are supposed to work harder, be nicer, and make sure to avoid burnout. The organization simply must reduce overall workload on all participants.” —Physician Provide Better Pay “ Hire appropriate and well-trained staff, and pay staff whatever is appropriate for their level of knowledge and the patient care they provide . This organization pays travelers four times what in-house staff gets paid, and 90% of the time, we have to do a chunk of the travelers’ workload. There are few incentives to stay within this organization.” —Nurse “ Safe staffing needs to be a top priority, in addition to fair compensation for workload . The organization should hire more staff to be able to adequately care for patients.” —Nurse What Is the KLAS Arch Collaborative? The Arch Collaborative is a group of healthcare organizations committed to improving the EHR experience through standardized surveys and benchmarking. To date, over 300 healthcare organizations have surveyed their end users and over 440,000 clinicians have responded. Reports such as this one seek to synthesize the feedback from these clinicians into actionable insights that organizations can use to revolutionize patient care by unlocking the potential of the EHR.

 "Without data, you're just another person with an opinion."
"Without data, you're just another person with an opinion."




 See Sample Benchmark Survey
See Sample Benchmark Survey





















